How is your gut microbiome connected to oestrogen metabolism
Oestrogen is a critical hormone for overall health—not only for reproductive function, but also
for immune regulation, brain function, and gut integrity. While both women and men require
healthy levels of endogenous estrogens, imbalances can lead to a variety of health challenges,
particularly when the gut microbiome is compromised.
Why Oestrogen Balance Matters
Low estrogen levels are associated with negative outcomes in immune and cognitive function,
gut health, and fertility. 1,2 On the other hand, excess or poorly metabolized estrogen—whether
from internal production or external exposure—can increase the risk of hormone-related
conditions such as breast cancer, endometriosis, and thyroid nodules.
Synthetic estrogens from oral contraceptives and xenoestrogens from plastics, cosmetics, and
household products further compound the issue.
The Gut Microbiome and Oestrogen Metabolism
The gut plays a surprisingly significant role in regulating estrogen through a group of bacterial
genes called the oestrobolome. The oestrobolome encodes enzymes—particularly Beta-
glucuronidase—that help to deconjugate estrogen, and I’ll discuss this more in the Understand
Your Tests section below.
This reactivation process must be tightly regulated. If β-glucuronidase activity is too high due to
dysbiosis (imbalance of the gut flora) or poor gut function, excess estrogen may recirculate,
potentially leading to oestrogen dominance or related health conditions.
Research shows that disruptions to the gut microbiota and oestrobolome function are linked
to oestrogen-related disorders, including:
Breast and endometrial cancer
Polycystic ovarian syndrome (PCOS)
Fibroids and endometriosis
Thyroid nodules
What is Oestrogen Dominance?
Estrogen dominance refers to an excess or relative excess of estrogen, either due to:
Elevated estrogen levels
Low progesterone
Impaired estrogen metabolism
So, you don’t need high oestrogen levels to be oestrogen dominant imbalances in how your
body processes estrogen or a drop in progesterone are still considered to be forms of estrogen
dominance.
Common Signs and Symptoms of Estrogen Dominance:
✔️Irregular or heavy periods
✔️Painful menstruation
✔️Breast tenderness
✔️Mood swings
✔️Bloating
✔️Fatigue
✔️Uterine fibroids
✔️Weight gain (especially around hips and thighs)
✔️Thyroid nodules
How to Test for Oestrogen Dominance
When a patient presents with symptoms of oestrogen dominance—or a history of fibroids,
endometriosis, or thyroid nodules—I often recommend a DUTCH test to assess oestrogen levels
and metabolism.
Markers evaluated include:
Estradiol (E2), Estrone (E1), and Estriol (E3)
2-OH, 4-OH, and 16-OH estrogen metabolites
Methylation capacity via 2-Methoxyestrone
A comprehensive stool panel can also be useful, especially if we suspect poor gut health or
elevated β-glucuronidase levels.
How to Address Oestrogen Dominance
To address estrogen dominance, it’s essential to both optimize oestrogen metabolism and
improve gut health:
✅ Eat foods that support oestrogen detoxification:
Cruciferous vegetables (e.g., broccoli, broccoli sprouts, cauliflower, kale)
Flaxseeds and chia seeds
High-fibre foods to promote regular elimination
✅ Support the gut microbiome:
Eat fermented foods like sauerkraut
Take probiotic and prebiotic supplements
Avoid processed foods and excessive sugar
✅ Take supportive supplements:
DIM (Diindolylmethane) for healthy estrogen metabolism (as long as estrogen levels aren't too
low)
Calcium-D-glucarate to lower β-glucuronidase
Methylated B vitamins to support estrogen metabolism
Magnesium and liver-support herbs (e.g., milk thistle)
✅ Reduce xenoestrogen exposure:
Choose glass or stainless steel over plastic
Use clean skincare and household products
Filter your drinking and shower water
✅ Consider advanced testing:
Comprehensive stool analysis
SIBO testing if bloating and gas are present
Hormone panels beyond the DUTCH test if warranted
Conclusion
Oestrogen imbalances are more than a hormonal issue—they’re often a gut issue too. The gut
microbiome directly affects how oestrogen is metabolized and cleared, and when the microbiome
is out of balance, symptoms of estrogen dominance can emerge—even if estrogen levels appear
“normal.”
By supporting gut health, reducing toxic exposures, and improving oestrogen detox pathways,
you can restore balance and reduce your risk of estrogen-related conditions.
Understand your tests
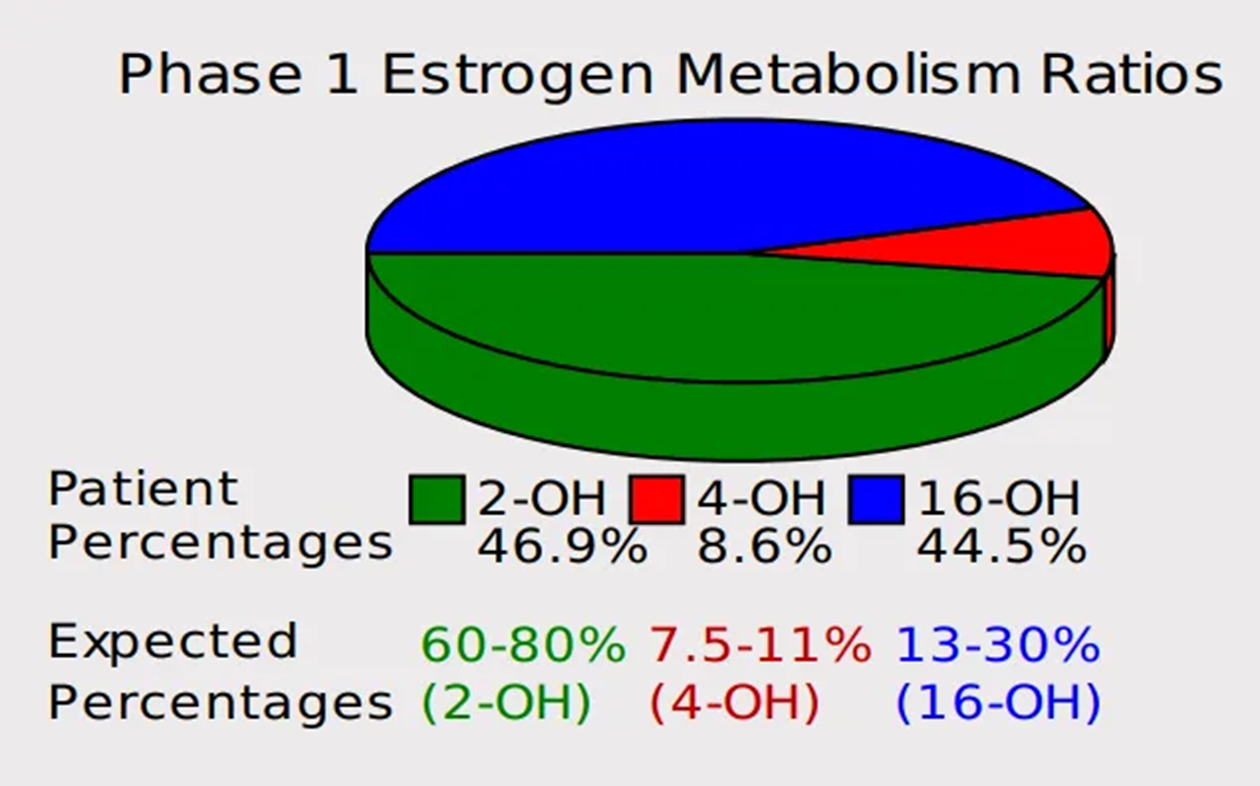
Patient Test #1: Elevated 4-OH metabolite levels
Patient Test #2: Elevated 16-OH metabolite levels
Patient Test #3: Beta-Glucuronidase
Markers Related to Oestrogen Metabolism
There are several ways to evaluate estrogen metabolism, with the most direct method
being the assessment of oestrogen metabolites via dried urine testing. The DUTCH test is
the most widely used tool for this purpose. It measures key estrogen metabolites, including:
2-Hydroxyestrone (2-OH)
4-Hydroxyestrone (4-OH)
16α-Hydroxyestrone (16-OH)
Interpreting oestrogen Metabolites
Ideally, 2-OH should be the most predominant metabolite, as it is considered the “cleanest”
oestrogen detoxification pathway. Elevated levels of 4-OH (Patient Test #1) or 16-OH
metabolites (Patient Test #2) can be problematic, as these pathways are associated with
increased oxidative stress and potential estrogen-related health risks.
If either the 4-OH or 16-OH metabolites are elevated, it is important to support oestrogen
metabolism through dietary and lifestyle strategies—such as increasing cruciferous
vegetables, taking DIM (diindolylmethane), and reducing xenoestrogen exposure—as outlined
in the main section.
Beta-Glucuronidase: An Indirect Marker
Another important, though indirect, marker of oestrogen metabolism is Beta-glucuronidase
(Patient Test #3), which I briefly mentioned earlier.
This enzyme is measured on certain comprehensive stool panels, including the GI-MAP
and GI Effects tests.
Elevated beta-glucuronidase activity may indicate intestinal dysbiosis, or an imbalance in the
gut microbiota. High levels of this enzyme can impair the glucuronidation pathway, which is
responsible for the detoxification and elimination of oestrogens. When beta-glucuronidase is
elevated, it can lead to the reabsorption of oestrogen, increasing the risk of oestrogen
dominance and related symptoms or conditions.